Lee Fisher is an Assistant Professor of Physical Medicine and Rehabilitation and Bioengineering at the University of Pittsburgh.
His research works to restore sensory and motor function after neural damage or disease. Recently, he was awarded the 2021 Krishna Kumar New Investigator Award by the North American Neuromodulation Society for his work on restoring somatosensory feedback to upper-limb amputees. Landan Mintch and Annie Rauwerda from Ripple Neuro sat down with him over Zoom* to discuss his career, the future of neuroprosthetics, and more! Be sure to attend his talk at this years 2021 NANS mid-year meeting.

*This transcription of the interview has been lightly edited for clarity.
Mintch: Thanks for joining us! Tell us, in your words, what you do in your lab.
Dr. Fisher: We work to improve the functionality of prosthetic limbs. Specifically, we work with people who have had either arm or leg amputations and incorporate sensory feedback into prosthetic limbs using electrical stimulation. This work involves implanting electrodes in the neck or lower back and then presenting stimulation that mimics that of a missing limb. Sensors on prosthetic limbs detect pressure and we use that information to send a message to the brain. For example, when the heel of the prosthetic limb strikes the ground, sensors will relay that information to a stimulator so the user can feel pressure in their missing foot. The goal is to make these systems available to anyone with a missing limb. This sensory feedback can also decrease phantom limb pain, which is experienced by about 85% of amputees.
Mintch: You got involved with neuroprosthetics during your PhD at Case Western, which you finished in 2012. How did you get involved in the field?
Dr. Fisher: My undergrad was in biomedical engineering at Boston University. For my senior project, I worked with Jim Collins. He’s a person who goes into a field, revolutionizes it, gets bored, and moves onto a new field. He’s a MacArthur Genius fellow– an amazing guy. He was working on vibrating shoe insoles to improve balance control for people with diabetes, the elderly, or other people who could benefit from increased sensory function. The project involved stochastic resonance— you boost weak signals so that they can be detected. That project lit the fire for neural engineering, and I attended Case Western’s PhD program the next year.
Mintch: Besides research, what are some classes you took that inspired you?
Dr. Fisher: The curriculum around neuroprosthetics at Case is amazing. When I was there, it was heavily focused on stimulation, not recording– which was great– because that’s what I was working on. I was taught by the leading researchers in the field, like Tom Mortimer, Dominique Durand, Dustin Tyler, and Bob Kirsch. A class on bioelectric phenomena– really, it was a math class– focused on understanding the effects of electric fields on neural tissue. That class was huge for me.
Mintch: Case Western was such an early leader in the neural engineering field.
Dr. Fisher: Yeah. Tom Mortimer did spinal cord stimulation in people in the sixties. There had been active research there for many decades.
Mintch: What are some recent developments in neuroengineering which excite you?
Dr. Fisher: A lot of people focus on things like brain computer interfaces and restoring function to those with spinal cord injury, and other lofty, high-tech approaches. To be clear, those efforts are really cool and worthwhile. But from a practical standpoint, I’m excited about other initiatives that could have much broader and more immediate effects, like restoring bladder function or treating disorders of internal organs. In certain situations, we can move away from pharmaceuticals and treat nervous system disorders with electrical stimulation. This movement toward “bioelectric medicine” might not be what first comes to mind when you think about neuroengineering, but it’s likely to have the most impact soon.
Mintch: Bioelectric medicine is a term that’s come up recently. What are your thoughts?
Dr. Fisher: I’m totally okay with it. It encapsulates what we do for people who might not know all the details. “Electroceuticals” is also used sometimes.
Mintch: Your recent paper was highlighted by a NANS Krishna Kumar award. It’s focus was on restoring sensory feedback via closed-loop electrical stimulation protocols. Do you see your work impacting other closed-loop stimulation applications?
Dr. Fisher: I work in a fairly unique lab environment. It’s the Rehab Neural Engineering Labs (RNEL), and within our group, many technologies are shared. In our spinal cord stimulation research, we use a lot of software and tools that were developed for brain computer interfaces. We develop new tools and then share them back to our colleagues. We made a new user interface in Python that shows hands or feet and allows patients to use sliders or checkboxes to identify what they’re feeling where. We open-sourced it and made it available, and other researchers have already started to use it. That’s an open-loop approach, but it speaks to the concept. I don’t want my work to be kept a secret. We’re working on a manuscript focused on a closed-loop experiment and once the paper is out the door, we’ll release the code. Hopefully it lowers the barrier to entry for researchers.
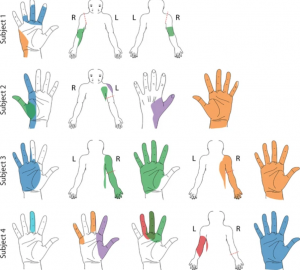
A figure taken from the publication illustrating the Python interface tool for patient selection of projected fields. “Colored areas represent selected projected fields that were reported for more than two testing sessions and remained stable for at least two weeks. Each color represents a unique stimulation electrode per subject.”
Mintch: There isn’t a lot of software that make closed-loop easy to do.
Dr. Fisher: Yeah. The goal is to set up our systems in a way that’s easy to reproduce so that we can change that.
Mintch: One of the cool things in the paper was mapping where sensory precepts are happening in the patients. I was surprised by the variability from patient to patient. Do you have any ideas for why patients can have such different reactions?
Dr. Fisher: Dermatomes (the regions of skin that receives sensations from a certain spinal nerve) are often oversimplified in diagrams. In real life, there is a lot of variability from person to person in how nerves map. You can have an electrode in the same anatomical location in two different people, and it can have very different effects. Because our subjects are awake when we place electrodes– we just use local anesthesia– they can tell us what different electrodes make them feel. Multipolar stimulation seems to allow more focal stimulations than unipolar, although in two of the four subjects, even if we could get a sensation localized to a finger, we would get sensations at the end of their residual line as well. We tried to get rid of that residual limb sensation, and we couldn’t. There’s a lot of discussion in the field about how sensory remapping happens after an amputation, and this result suggests that the residual limb of the amputation might be given more sensory weight than, say, the areas in the missing limb. One thing we’re working on is getting smaller electrodes, which might lead to more focal sensations.
Mintch: Is electrode geometry your biggest issue?
Dr. Fisher: Hm, I’d also like better stimulators! We don’t really have an implantable stimulator that does the things we need it to do. The current stimulators approved for use for spinal cord stimulation are made to be used at a constant level all day, not to be rapidly adjusted. I wish we could adjust stimulation every 20 milliseconds. Currently, we only do percutaneous studies, but whenever electrodes come through the skin, we have to be careful not to leave them in too long due to infection risk. We only leave electrodes in for 29 days, which limits the amount of data we can collect and doesn’t give us enough time to look at plasticity. Moving to implanted stimulation technology will be huge.
Mintch: We know that a common reason for prosthesis abandonment is lack of somatosensory feedback. You and many others are working to change that. What are some other challenges in prosthetic limbs?
Dr. Fisher: Sockets are always going to be a problem. They’re usually uncomfortable and annoying throughout the day as people sweat and live their lives. Osseointegration is a really exciting field right now. Motor function has room for improvement too. There are many basic functions that prosthetic limbs can’t do, like picking up a coin or lighting a match. There are a lot of bottlenecks that we’re working on in parallel right now.
Rauwerda: It’s so exciting to see so much progress happening right now in neuroprosthetics. We have a few more questions that are less focused on research. First up, if you could design your own class to teach right now, what would it be?
Dr. Fisher: I’d be interested in exploring neuroethics as well as diving into equity and access to neuroprosthetics. How do we make sure we’re engaging with everybody in the way we design our devices? I’d like to think more broadly and less technically about the way we design our devices. Some students and postdocs in our lab run a monthly neuroethics series which is really interesting.
Rauwerda: Of all the places you’ve worked, which had the best view out of the window?
Dr. Fisher: Definitely not grad school, when I worked in a basement. My office is in Pittsburgh in a pretty densely populated area, and I can look out at the city. Working from home isn’t too bad either.
Rauwerda: How has working from home been for you?
Dr. Fisher: It’s been a tough time, but some aspects are great. I like having time away from distractions where I can sit down and write, for example. It’s great to have chunks of time free from meetings.
Rauwerda: If you could give advice to your 18-year-old self, what would it be?
Dr. Fisher: Things work out. If you work hard and are willing to go for the ride, you’ll end up okay.
Rauwerda: What’s something you’ve read recently that you’d recommend?
Dr. Fisher: I’m a big Stephen King fan. I recently got my wife to read his Dark Tower series, seven books that are his big opus. They’re excellent.
This is the conclusion of this interview! Ripple would like to thank Dr. Fisher for taking time out of his busy schedule to let us pick his brain a bit about his recent work and wish him all the best in his future projects!

